The pelvic floor plays a central role in women’s health by maintaining core stability and regulating bladder, bowel, and sexual function. When these muscles are impaired, the effects can be widespread, impacting comfort, daily mobility, and recovery after childbirth. Fortunately, early recognition and treatment can restore function and improve long-term health.
Many women experience pelvic floor issues without realizing that effective treatment options exist. Pelvic floor rehabilitation offers targeted support to restore strength, improve muscle coordination, and enhance daily comfort. With personalized care plans and evidence-based approaches, women can regain confidence and long-term pelvic health.
What is the Pelvic Floor, and Why is it Important?
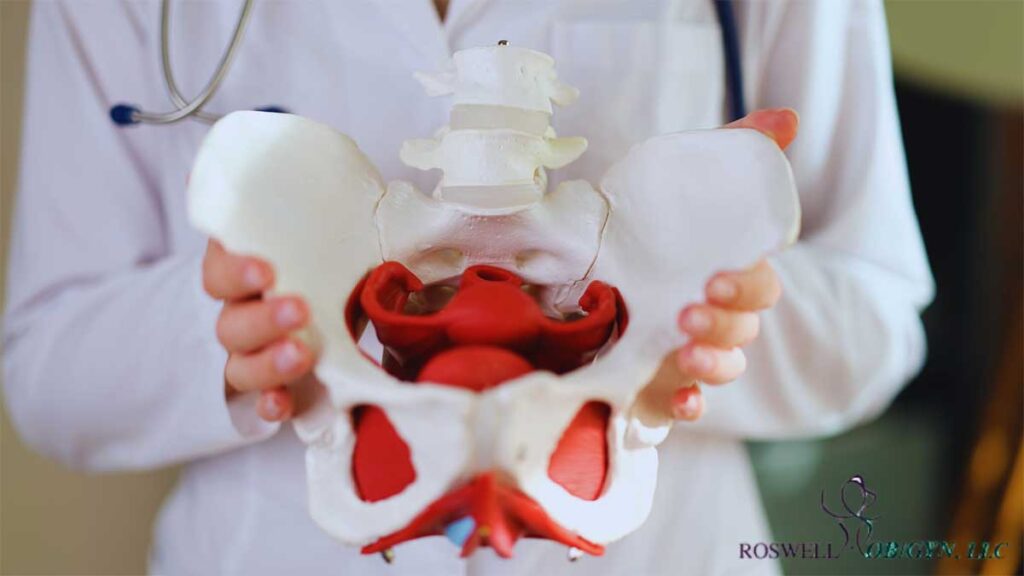
The pelvic floor is a group of muscles, ligaments, and connective tissues that form a supportive sling at the base of the pelvis. These muscles play a critical role in controlling some of the body’s most essential functions—including urination, bowel movements, core stability, and sexual performance. Acting like a hammock, the pelvic floor supports the bladder, uterus (in women), rectum, and other pelvic organs, ensuring they stay in place and function properly.
When the pelvic floor muscles are working well, they contract and relax in harmony with the body’s needs. This allows for effective bladder and bowel control, supports movement and posture, and contributes to pleasurable and pain-free sexual activity. But if these muscles become too weak or too tight, it can disrupt normal function and lead to a range of problems.
The Impact of Pelvic Floor Health on Overall Well-Being
Pelvic floor dysfunction affects more than just bladder control. It can have far-reaching consequences on physical, emotional, and sexual health. A weakened or overly tight pelvic floor can disrupt daily activities, cause chronic pain, and significantly impact mental well-being.
Many women delay seeking treatment due to embarrassment or lack of awareness, but early intervention can prevent symptoms from worsening. Recognizing the link between pelvic floor health and overall well-being is the first step in prioritizing care and exploring effective treatment options.
Can a Weak Pelvic Floor Cause Other Health Problems?
Weak or dysfunctional pelvic floor muscles may lead to broader musculoskeletal issues. These include lower back and hip pain due to instability, as well as sexual dysfunction from poor muscle coordination or chronic tension. Early therapeutic intervention helps prevent long-term strain on surrounding structures and reduces discomfort over time.
Potential Complications of Pelvic Floor Dysfunction Include:
- Lower Back and Hip Pain: Instability in the pelvic floor can strain surrounding joints and muscles, leading to chronic discomfort, poor posture, and mobility limitations.
- Sexual Dysfunction: Muscle imbalance or tightness may result in pain during intercourse (dyspareunia), decreased sensitivity, or difficulty with orgasm.
- Chronic Pelvic Pain: Persistent tension or weakness in the pelvic region can cause ongoing pain in the lower abdomen, hips, or tailbone, sometimes mistaken for gastrointestinal or gynecological conditions.
Comprehensive evaluation and pelvic floor rehabilitation can restore function, improve comfort, and reduce the risk of long-term complications.
How Does Pelvic Floor Health Affect Quality of Life?
Pelvic floor dysfunction doesn’t just affect the body. It impacts mental and emotional well-being as well. Women experiencing incontinence, pelvic pressure, or sexual discomfort often feel embarrassed, anxious, or even socially withdrawn.
The Emotional and Psychological Effects of Pelvic Floor Dysfunction
- Loss of Confidence Fear of bladder leaks or discomfort can lead to self-consciousness and avoidance of social activities, exercise, or intimacy.
- Increased Stress and Anxiety Worrying about symptoms can trigger emotional distress, making it harder to focus on daily tasks or engage in relationships.
- Reduced Sexual Well-Being Pain or discomfort during intimacy can lead to avoidance of physical closeness, relationship strain, or decreased sexual satisfaction.
- Sleep Disruptions Frequent nighttime urination (nocturia) due to weak bladder control can impact sleep quality and energy levels, leading to fatigue and irritability.
Benefits of Addressing Pelvic Floor Dysfunction Early
- Restored Comfort and Mobility Strengthening or relaxing the pelvic floor can eliminate pain, improve posture, and enhance physical movement.
- Improved Sexual Health Treating pelvic floor dysfunction can reduce pain, increase blood flow, and restore pleasurable sensations.
- Better Mental Health Managing symptoms helps reduce anxiety, boost confidence, and improve overall quality of life.
Ignoring pelvic floor symptoms can cause progressive worsening over time, making early diagnosis and intervention critical. Seeking care from an experienced OBGYN can restore function, relieve discomfort, and enhance overall well-being.
Recognizing Symptoms of Pelvic Floor Dysfunction
Pelvic floor dysfunction can manifest in subtle or disruptive ways, affecting bladder control, bowel movements, sexual health, and overall comfort. Many women dismiss early signs, assuming they are a normal part of aging, childbirth, or hormonal changes. However, identifying symptoms early can prevent long-term complications and chronic discomfort.
What Symptoms Indicate Pelvic Floor Issues?
Pelvic floor dysfunction presents with a range of symptoms depending on whether the muscles are weak, tight, or uncoordinated.
Common Signs of Pelvic Floor Dysfunction
- Urinary Urgency and Frequency: Feeling the need to urinate frequently or struggling to hold urine.
- Urinary Leakage (Incontinence): Leaking urine during physical activity, coughing, laughing, or sneezing.
- Painful Intercourse (Dyspareunia): Discomfort or pain during penetration, often linked to pelvic muscle tightness.
- Pelvic Pressure or Heaviness: A sensation of fullness, dragging, or something “falling” in the vaginal area, which may indicate pelvic organ prolapse.
- Difficulty emptying the bladder or bowel straining, incomplete emptying, or the need to reposition to urinate or defecate properly.
- Chronic Lower Back, Hip, or Pelvic Pain: Unexplained pain in these areas may be due to pelvic muscle dysfunction, nerve irritation, or structural imbalances.
Because pelvic floor dysfunction presents differently in every woman, it is important to pay attention to recurring symptoms and seek medical advice if discomfort persists.
How is Pelvic Floor Health Assessed?
Diagnosing pelvic floor dysfunction requires a thorough evaluation to determine muscle strength, coordination, and any underlying conditions contributing to symptoms. A comprehensive OBGYN assessment helps identify the root cause and create a personalized treatment plan.
Key Components of a Pelvic Floor Evaluation
- Physical Examination: Assessing muscle tone, coordination, and reflexes to determine weakness, tightness, or imbalances.
- Symptom History: Discussing bladder, bowel, and sexual function, along with any past pregnancies, surgeries, or injuries that may impact pelvic health.
- Diagnostic Tests: If needed, imaging studies (ultrasound, MRI) or biofeedback assessments may be used to measure muscle activity and pinpoint dysfunction.
A proper diagnosis is the first step in developing a targeted treatment strategy. With the right approach, pelvic floor dysfunction is highly treatable, improving physical function, reducing pain, and restoring confidence.
Strengthening and Treating Pelvic Floor Dysfunction
Pelvic floor dysfunction often improves with individualized treatment. Strength-focused exercises, guided rehabilitation, and supportive therapies address both pain and weakness to restore comfort and mobility.
What Exercises Improve Pelvic Floor Strength?
Pelvic floor exercises are essential for strengthening and restoring muscle function, but proper technique is key. Doing the wrong exercises or engaging the wrong muscles can worsen symptoms. Your OBGYN can guide you through a personalized rehabilitation plan to ensure proper technique and results.
Recommended Exercises for Pelvic Floor Strength
- Kegel Exercises Strengthen the muscles responsible for urinary and bowel continence, pelvic support, and sexual function.
- Diaphragmatic Breathing Helps relax and coordinate pelvic muscles, reducing tension and improving core-pelvic synergy.
- Core Stabilization Movements Strengthen deep abdominal muscles, improving posture, stability, and pelvic floor support.
While home exercises are beneficial, professional guidance ensures proper activation of the pelvic muscles without overcompensation from surrounding areas. Pelvic floor rehabilitation plans are tailored by your OBGYN to match your individual needs, including strength, flexibility, and coordination.
Are There Specific Treatments for Pelvic Floor Dysfunction?
Pelvic floor dysfunction is treatable through targeted rehabilitation designed to restore muscle control, relieve discomfort, and improve quality of life. At Roswell, care plans are guided by experienced OBGYNs who assess your symptoms, identify underlying causes, and provide structured rehabilitation tailored to your needs.
Pelvic floor rehabilitation may include:
- Manual techniques to ease muscle tension, support healing, and promote flexibility
- Biofeedback-based strategies to improve awareness and coordination of pelvic muscles
- Electrical stimulation to help activate and strengthen weakened muscle groups
- Lifestyle guidance to address contributing factors such as diet, hydration, and posture
When necessary, your OBGYN may also discuss additional interventions such as medication or minimally invasive procedures. Early, comprehensive care ensures better outcomes and long-term pelvic health.
Pelvic Floor Health During Pregnancy and Postpartum
During pregnancy and postpartum, the pelvic floor endures increased strain due to weight gain, hormonal changes, and labor. These shifts can weaken muscle tone, increase discomfort, and contribute to postpartum challenges.
How Can Pregnancy Affect Pelvic Floor Health?
The added pressure from a growing uterus and the physical demands of childbirth can compromise pelvic floor stability. Without focused rehabilitation, symptoms like incontinence or pelvic discomfort may persist beyond delivery. Preventive care during this time helps protect long-term pelvic function.
Can a Gynecologist Help with Pelvic Floor Issues?
OBGYNs play a central role in evaluating and treating pelvic floor dysfunction, especially during pregnancy and the postpartum period. By identifying issues early, they help prevent complications that could affect long-term comfort and function.
How an OBGYN Can Help:
- Perform Pelvic Screenings: Assess for signs of muscle weakness, tightness, or prolapse during routine visits.
- Provide In-Office Pelvic Floor Rehabilitation: Develop customized rehabilitation plans to improve muscle control, relieve symptoms, and support healing.
- Offer Postpartum Support: Monitor recovery progress and address any concerns related to bladder control, core stability, or pelvic discomfort.
Prioritize Your Pelvic Health Today
Pelvic floor dysfunction is a treatable condition that can significantly impact daily life. Seeking professional care early can restore strength, improve function, and prevent long-term complications. If you are experiencing pelvic discomfort, incontinence, or postpartum recovery challenges, expert intervention can provide lasting relief.
Roswell Ob/Gyn, LLC offers comprehensive pelvic floor rehabilitation tailored to your unique needs. Our experienced team provides expert evaluation, evidence-based treatments, and personalized care to help you regain control and confidence. Schedule a consultation today and take the next step toward a stronger, healthier pelvic floor.