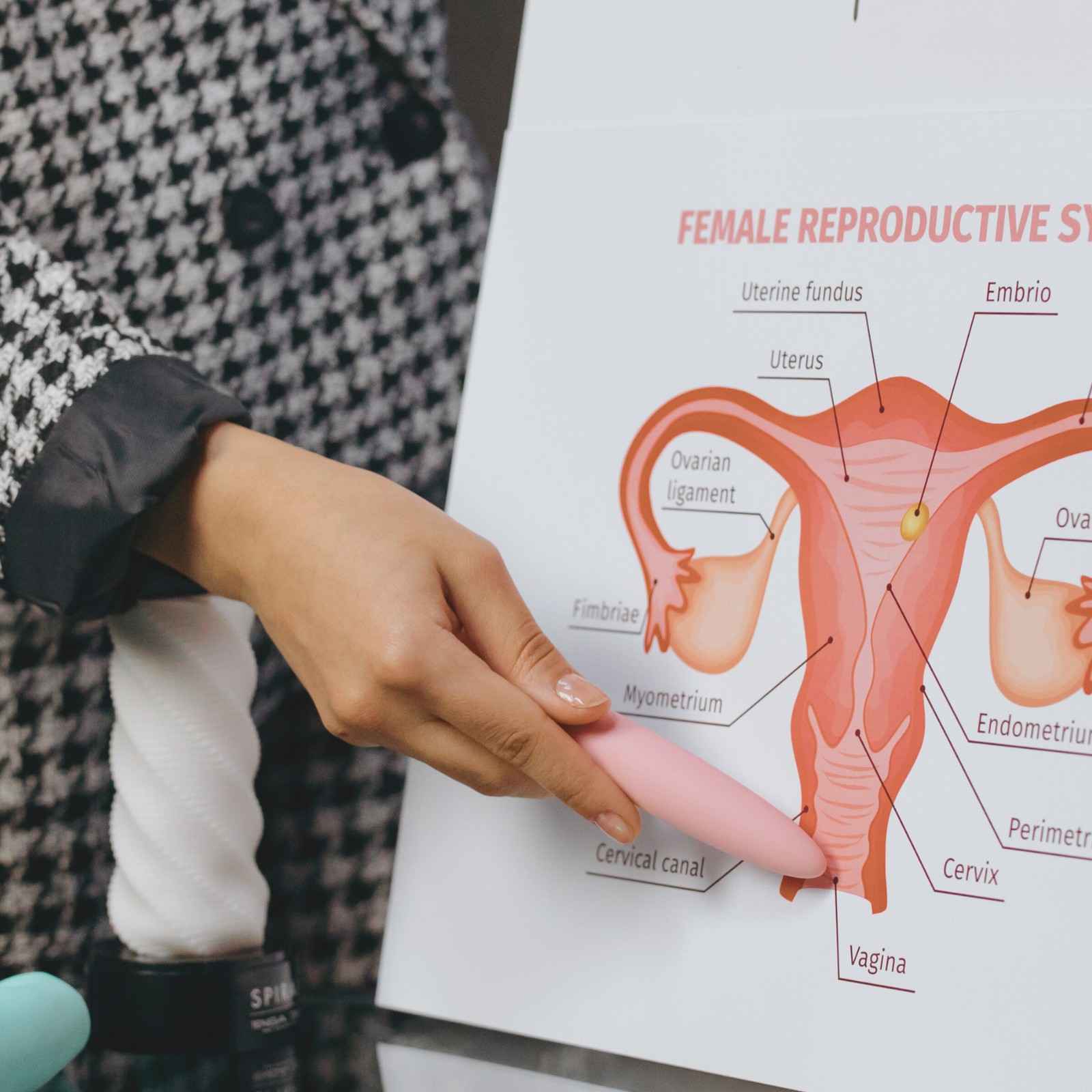
Chronic vulvar pain affects many of us, yet it often goes undiagnosed for years. Vulvodynia is a complex condition characterized by persistent discomfort in the vulvar area (the external part of the genital region) without an identifiable cause like infection or skin disease. If you experience ongoing vulvar discomfort, talking with an OBGYN can help you understand what you’re feeling and rule out other conditions. Below, we’ll walk through the possible causes, symptoms, and treatment options that may help you find relief.
What Is Vulvodynia?
Vulvodynia refers to chronic vulvar pain lasting three months or longer without visible signs of infection, injury, or other gynecological problems. This condition affects the external female genitalia and can impact your quality of life, but effective treatments help many patients find significant relief. Research suggests approximately 16% of women experience vulvodynia at some point, so you’re not alone in seeking answers.
Types of Vulvodynia
Gynecology specialists classify vulvodynia into two main categories based on when pain occurs:
Provoked vulvodynia (vestibulodynia):
- Happens in response to touch or pressure
- Triggered by intercourse, tampon use, pelvic exams, tight clothing, or prolonged sitting
Unprovoked (spontaneous) vulvodynia:
- Occurs without direct contact or stimulation
- Involves constant or intermittent burning lasting hours or days
Some women experience both types, with symptoms varying throughout the day or month. Pain can concentrate in one area, like the vaginal opening, or spread across the entire vulvar region. Your provider identifies your specific pattern to determine the most effective treatment approach.
Common Symptoms You May Experience
Most women describe sensations of burning, stinging, rawness, soreness, throbbing, or itching that don’t respond to typical treatments. Symptoms may intensify with certain activities like sitting, exercise, or intimacy, though intensity varies considerably. Some describe it as feeling like a constant sunburn or paper cut, while others experience episodes with pain-free periods between.
Your experience is valid, and we can work together to develop a treatment plan that improves your comfort.
How Vulvodynia Differs from Other Conditions
Several conditions share similar symptoms but require different treatments. Yeast infections produce discharge and visible inflammation, bacterial vaginosis creates distinct odor and discharge, lichen sclerosus causes visible white patches, herpes produces visible lesions, and contact dermatitis shows apparent skin irritation. Vulvodynia causes pain without these visible signs or positive infection tests.
An experienced OBGYN performs thorough testing to ensure accurate diagnosis, then focuses on treatments designed explicitly for nerve-related vulvar pain.
What Causes Vulvodynia?
The exact cause of vulvodynia remains under investigation; however, research suggests multiple contributing factors that inform practical treatment approaches tailored to your specific situation. Understanding these mechanisms provides reassurance that your symptoms have identifiable physiological origins rather than being “all in your head” as some women unfortunately hear. These factors combine differently for each woman, which is why personalized management strategies are more effective than one-size-fits-all approaches.
Nerve Sensitivity and Pain Signals
Nerve sensitivity is a common factor in vulvodynia, where nerves in the vulvar area send heightened pain signals in response to stimuli. This heightened nerve response can develop after repeated yeast infections, urinary tract infections, injury during childbirth, surgical procedures in the pelvic area, or prolonged use of topical medications. These nerves may remain hypersensitive even after the initial trigger resolves, similar to other chronic pain conditions.
Effective approaches specifically target nerve hypersensitivity and help retrain your nervous system to process signals more appropriately. Nerves can adapt and become less reactive over time with proper treatment, and many patients experience meaningful improvement in their symptoms.
Pelvic Floor Dysfunction
Your pelvic floor muscles support your bladder, uterus, and rectum. When these muscles become too tight, weak, or dysfunctional, they can contribute to vulvar pain. Chronic muscle tension creates persistent pressure on vulvar nerves, triggering pain signals even during routine activities. This dysfunction often develops through chronic stress, previous pelvic trauma or surgery, poor posture, or unconscious muscle guarding.
Pain and muscle tension can create a self-reinforcing cycle that requires specialized pelvic floor rehabilitation to break. Physical therapy techniques help release tight muscles, improve coordination, and reduce muscle-generated pain without the need for medication or invasive procedures.
Hormonal and Inflammatory Factors
Hormonal changes may contribute to vulvodynia development, particularly fluctuations in estrogen, progesterone, and testosterone. Low estrogen levels can cause vaginal dryness and tissue thinning, especially during perimenopause, after childbirth, or during specific hormonal treatments. Some women notice symptom changes related to their menstrual cycle, which we can sometimes address through targeted hormone therapy.
Inflammatory processes may also play a role. Research shows elevated inflammatory markers in some women with vulvodynia, and certain autoimmune conditions may increase risk. Many women with hormonal or inflammatory factors respond well to treatments addressing these specific contributors.
ALSO READ: Pelvic Organ Prolapse: Signs and Solutions
How Is Vulvodynia Diagnosed?
A thorough evaluation by a knowledgeable provider confirms that your pain is real and can be effectively treated. This comprehensive evaluation ensures you receive appropriate treatment for your specific situation.
Your Initial Gynecology Appointment
Your first appointment involves discussing your symptoms, medical history, and how pain affects your daily life in a supportive environment. We ask about the onset and progression of pain, what triggers or worsens symptoms, and any previous treatments you’ve tried. Many women feel embarrassed discussing vulvar pain, but OBGYN specialists regularly address these concerns and understand the significant impact on their well-being.
This conversation guides our examination and testing approach while ensuring you feel heard.
Physical Examination and Testing
Your provider performs a gentle examination to assess skin changes, areas of tenderness, muscle tension, and patterns of pain location. The cotton swab test involves gently touching different vulvar areas to map where you feel pain and its intensity. We collect samples to test for yeast, bacterial, and sexually transmitted infections.
Your provider moves at your pace and stops immediately if you need a break. The goal is to gather necessary information while respecting your comfort at all times.
Ruling Out Other Conditions
Proper diagnosis involves systematically excluding other causes through cultures for infections, pH testing, blood work for hormonal levels or autoimmune markers if indicated, and occasionally a biopsy if unusual skin changes appear. Your OBGYN will explain each test and the reasons for our recommendation. Once we establish a precise diagnosis, we can move forward confidently with targeted treatments.
What Treatment Options Are Available?
Vulvodynia treatment requires a multifaceted approach tailored to your specific symptoms and contributing factors, with many patients finding symptom relief through a combination of treatments rather than a single intervention.
Obstetrics and Gynecology specialists work together to create personalized management strategies addressing all aspects of your condition. Our team offers a range of treatment approaches tailored to your needs, and if one approach doesn’t work well for you, we have others to try until we find what brings you relief.
Medication-Based Approaches
Several medication categories help manage vulvodynia symptoms by addressing nerve hypersensitivity, hormonal factors, or pain signals. Your provider may adjust dosages or try different combinations to find what works best for you. Most nerve-modifying medications require several weeks to show benefit, so patience during the initial treatment phase helps ensure you experience their full potential.
Topical treatments:
- Lidocaine ointment for numbing before activities that trigger pain
- Estrogen cream to address hormonal factors and tissue health
- Compounded medications combine multiple therapeutic ingredients
Oral medications:
- Tricyclic antidepressants in low doses to reduce nerve pain
- Anticonvulsants such as gabapentin to calm overactive nerves
- Pain relievers for symptom management during flare-ups
Physical Therapy and Pelvic Floor Rehabilitation
Specialized pelvic floor physical therapy addresses muscular components of vulvodynia through techniques that release tight muscles, improve coordination, and reduce muscle-generated pain. This treatment option carries no side effects and provides you with the skills to manage your condition in the long term. Most women attend therapy once or twice a week for several weeks, then gradually reduce the frequency as they learn maintenance techniques.
A trained therapist teaches you specific approaches:
- Internal and external manual therapy
- Biofeedback to increase muscle awareness
- Exercises for relaxation and strengthening
- Electrical stimulation for muscle reeducation
The hands-on nature of this treatment allows your therapist to target specific tight areas while teaching you maintenance techniques to use between sessions.
ALSO READ: Signs of Hormonal Imbalance in Women
Lifestyle Modifications and Self-Care
Daily habits and self-care practices support other treatments and help prevent symptom flares without requiring prescriptions or appointments.
| Category | Helpful Approaches |
| Clothing | Wear loose-fitting cotton underwear; avoid tight pants or synthetic fabrics; remove wet bathing suits or workout clothes promptly |
| Hygiene | Use only water or mild, fragrance-free cleansers; avoid douches, feminine hygiene sprays, or scented products; pat dry gently; use white, unscented toilet paper |
| Daily Activities | Use cushions when sitting for extended periods; take breaks during activities that trigger symptoms; apply cold packs for acute pain episodes |
| Intimacy | Use adequate lubrication; try different positions to reduce pressure; communicate openly with your partner about comfort levels |
These modifications work best alongside other treatments, but they provide practical strategies you can implement immediately while waiting for medications or therapy to take full effect.
Advanced Treatment Considerations
For cases not responding to initial treatments after 3-6 months, obgyn specialists may recommend more targeted approaches. Your provider discusses risks, benefits, and success rates to help you make informed decisions based on your individual situation.
Advanced options include:
- Nerve blocks to temporarily interrupt pain signals
- Botox injections to relax chronically tight pelvic floor muscles
- Vestibulectomy (surgical removal of painful tissue) for localized provoked vulvodynia
Most patients find symptom relief through standard treatments without needing these advanced options. We start with the least invasive approaches and progress toward more targeted interventions only when necessary, always prioritizing your comfort and daily function.
When Should You See an OBGYN Specialist?
Schedule an appointment if you experience vulvar pain or burning lasting more than three months, pain that interferes with daily activities or intimacy, discomfort during gynecological exams or tampon use, symptoms not improving with over-the-counter treatments, or pain accompanied by changes in urination or bowel movements.
Early evaluation and treatment often lead to better outcomes because addressing chronic pain promptly helps prevent nerve sensitivity from becoming more entrenched over time. Vulvodynia is a recognized medical condition deserving appropriate diagnosis and treatment.
Finding the Right Care at Roswell Ob/Gyn, LLC
At Roswell Ob/Gyn, LLC, our team understands the complex nature of vulvodynia and its impact on your life. We provide experienced obgyn specialists, personalized management strategies, coordination with pelvic floor physical therapists, and compassionate care in a respectful environment. Our approach combines medical expertise with genuine concern for your well-being, taking the time to listen to your concerns, answer your questions, and work collaboratively toward achieving your treatment goals.
We’ve helped many women manage vulvodynia successfully. Contact us today to schedule a consultation and begin your path toward lasting relief.